Clavicle Fractures
We treat all types of clavicle injury and have one of the largest experience in the world of intramedullary or nail treatment if clavicle fractures
- Fractures of the clavicle: an overview.
- Intramedullary fixation of diaphyseal clavicle fractures using the rockwood clavicle pin: review of 86 cases.
The trimodal distribution described by Allman is as follows:
- Group I: median age of 13 years, accounting for 76% of clavicular fractures.
- Group II: median age of 47 years, accounting for 21%.
- Group III: median age of 59 years, accounting for 3%.
Anatomy
- The clavicle is the first bone to ossify (fifth week of gestation) and the last ossification center (sternal end) to fuse at 22 to 25 years of age.
- It is the only long bone to ossify by intramembranous ossification without a cartilaginous stage.
- The clavicle is the only osseous strut connecting the trunk to the shoulder and arm.
- The flat outer third is the attachment site for the trapezius and deltoid muscles and the acromioclavicular and coracoclavicular ligaments.
- The tubular medial one-third protects the brachial plexus, the subclavian and axillary vessels, and the superior lung. It is strongest in axial load.
- The junction between the two cross-sectional configurations occurs in the middle third and constitutes a vulnerable area to fracture, especially with axial loading. Moreover, the middle third lacks reinforcement by muscles or ligaments distal to the subclavius insertion, resulting in additional vulnerability.
Mechanism of Injury
- No correlation exists between the fracture location and the mechanism of injury.
- Falls onto the affected shoulder account for most (87%) clavicular fractures, with direct impact accounting for only 7% and falls onto an outstretched hand accounting for 6%.
- Uncommonly, clavicular fractures occur with aberrant muscle contractions during seizures or atraumatically from pathologic mechanisms or stress fractures.
Evaluation
Clinical Evaluation
- The patient usually presents with splinting of the affected extremity, with the arm adducted across the chest and supported by the contralateral hand to unload the injured clavicle.
- A careful neurovascular examination is necessary to ensure the integrity of neural and vascular elements lying posterior to the clavicle.
- The proximal fracture end is usually prominent and may tent the skin. Crepitus may be present. Assessment of skin integrity is essential to rule out an open fracture.
- The chest should be auscultated for symmetric breath sounds. Tachypnea may be present due to pain with inspiratory effort; this should not be confused with diminished breath sounds, which may be present from an ipsilateral pneumothorax due to apical lung injury.
- Associated skeletal injuries, including head, neck, coracoid, acromioclavicular, sternoclavicular, scapulothoracic, and rib injuries, should be ruled out.
Radiographic Evaluation
- Proximal third fractures are uncommon and may represent epiphyseal injury if the sternal ossification center is not fused. An anteroposterior view and a 45-degree caudal tilt view may demonstrate injury.
- With middle third fractures, an anteroposterior view and a 45-degree caudal tilt view are usually sufficient to demonstrate the injury.
- With distal third fractures, standard radiographs typically overexpose the distal clavicle. In addition, evaluation of ligamentous integrity is essential. Neer recommends three views:
- Anteroposterior view of both shoulders with 10-lb weights strapped to the wrists: compare the distance between coracoid and medial fragments.
- Anterior 45-degree oblique: taken with the patient erect and the affected shoulder placed flat on the radiographic plate; provides lateral view of scapula and demonstrates the proximal fragment posteriorly and the distal fragment anteriorly.
- Posterior 45-degree oblique.
- Computed tomography may be useful in the evaluation of a fracture, especially in cases of proximal third fractures, to differentiate sternoclavicular dislocation from epiphyseal injury or in distal third fractures to identify articular involvement.
Classification
Descriptive Classification
Clavicle fractures may be classified according to anatomic description, including location, displacement, angulation, pattern (i.e., greenstick, oblique, transverse), and comminution.
Allman Classification
- Group I: fracture of the middle third (80%). Most common fracture in both children and adults; proximal and distal segments are secured by ligamentous and muscular attachments.
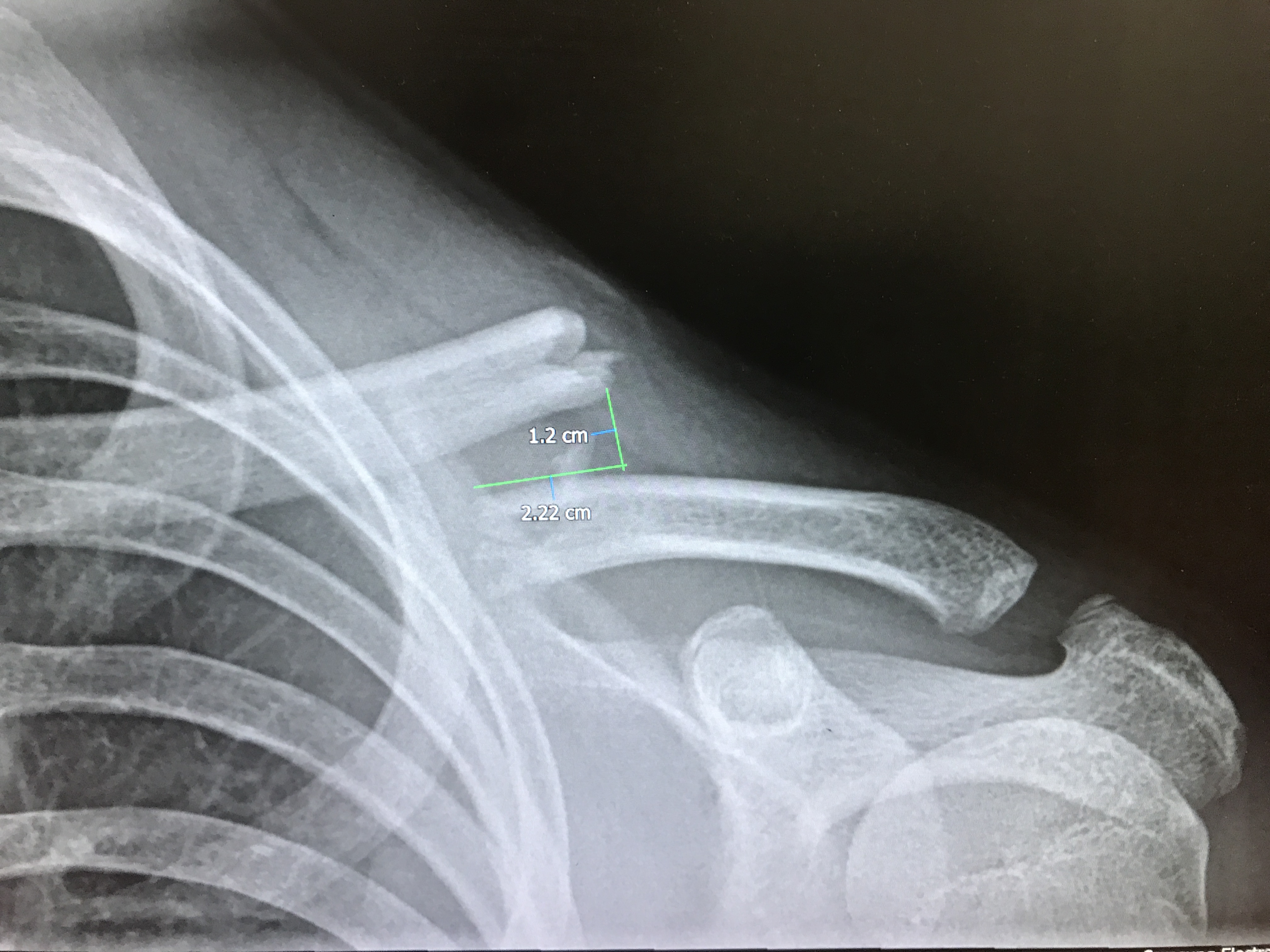
- Group II: fracture of the distal third (15%) (Figs. 9.1, 9.2, 9.3, 9.4). Subclassified according to the location of coracoclavicular ligaments relative to the fracture as follows:
- Type I: minimal displacement—interligamentous fracture between conoid and trapezoid or between the coracoclavicular and acromioclavicular ligaments (Fig. 9.1).
- Type II: displaced secondary to a fracture medial to the coracoclavicular ligaments—higher incidence of nonunion.
- IIA: conoid and trapezoid attached to the distal segment (Fig. 9.2)
- IIB: conoid torn, trapezoid attached to the distal segment (Fig. 9.3)
- Type III: fracture of the articular surface of the acromioclavicular joint with no ligamentous injury—may be confused with first-degree acromioclavicular joint separation (Fig. 9.4).
- Group III: fracture of the proximal third (5%). Minimal displacement results if the costoclavicular ligaments remain intact. May represent epiphyseal injury in children and teenagers. Subgroups include the following:
- Type I: minimal displacement.
- Type II: displaced.
- Type III: intraarticular.
- Type IV: epiphyseal separation.
- Type V: comminuted.
Orthopaedic Trauma Association (OTA)
Classification of Clavicle Fractures
- Clavicle fracture, medial end
- Type A: metaphyseal
- A1: extraarticular, impacted
- A2: extraarticular, displaced
- A3: extraarticular, multifragmentary
- Type A: metaphyseal
- Clavicle fracture, diaphyseal
- Type A: simple
- A1: spiral
- A2: oblique
- A3: transverse
- Type B: wedge
- B1: spiral wedge
- B2: bending wedge
- B3: fragmented wedge
- Type C: complex
- C1: spiral
- C2: segmental
- C3: irregular
- Type A: simple
- Clavicle fracture, lateral end
- Type A: extraarticular metaphysis
- A1: impacted
- A2: displaced (coracoclavicular ligaments intact)
- A3: multifragmentary (coracoclavicular ligaments intact)
- Type B: intraarticular
- B1: slight displacement (no dislocation)
- B2: wedge fracture with dislocation
- B3: multifragmentary fracture with dislocation
- Type A: extraarticular metaphysis
Treatment
Nonoperative Treatment
- The management goal is to brace the shoulder girdle with sling immobilization for 4 to 6 weeks to ensure adequate reduction while allowing for ipsilateral use of the elbow, wrist, and hand.
- Closed treatment is successful in most cases, with no need for reduction. Comfort and pain relief are the main goals. A sling has been shown to give the same results as figure-of-eight bandages, while providing more comfort and fewer skin problems.
Operative Treatment

- Operative intervention with stable fixation should be considered for the following:
- Open fractures;
- Fractures with associated neurovascular injury;
- Fractures with severe associated injuries, such as a flail chest with multiple rib fractures or a scapulothoracic dissociation;
- Group II, type II fractures—controversial because these have a high nonunion rate if treated closed;
- Cosmetic reasons, such as uncontrolled deformity due to malunion, although the resultant operative scar may result in greater cosmetic disturbance than the deformity itself.
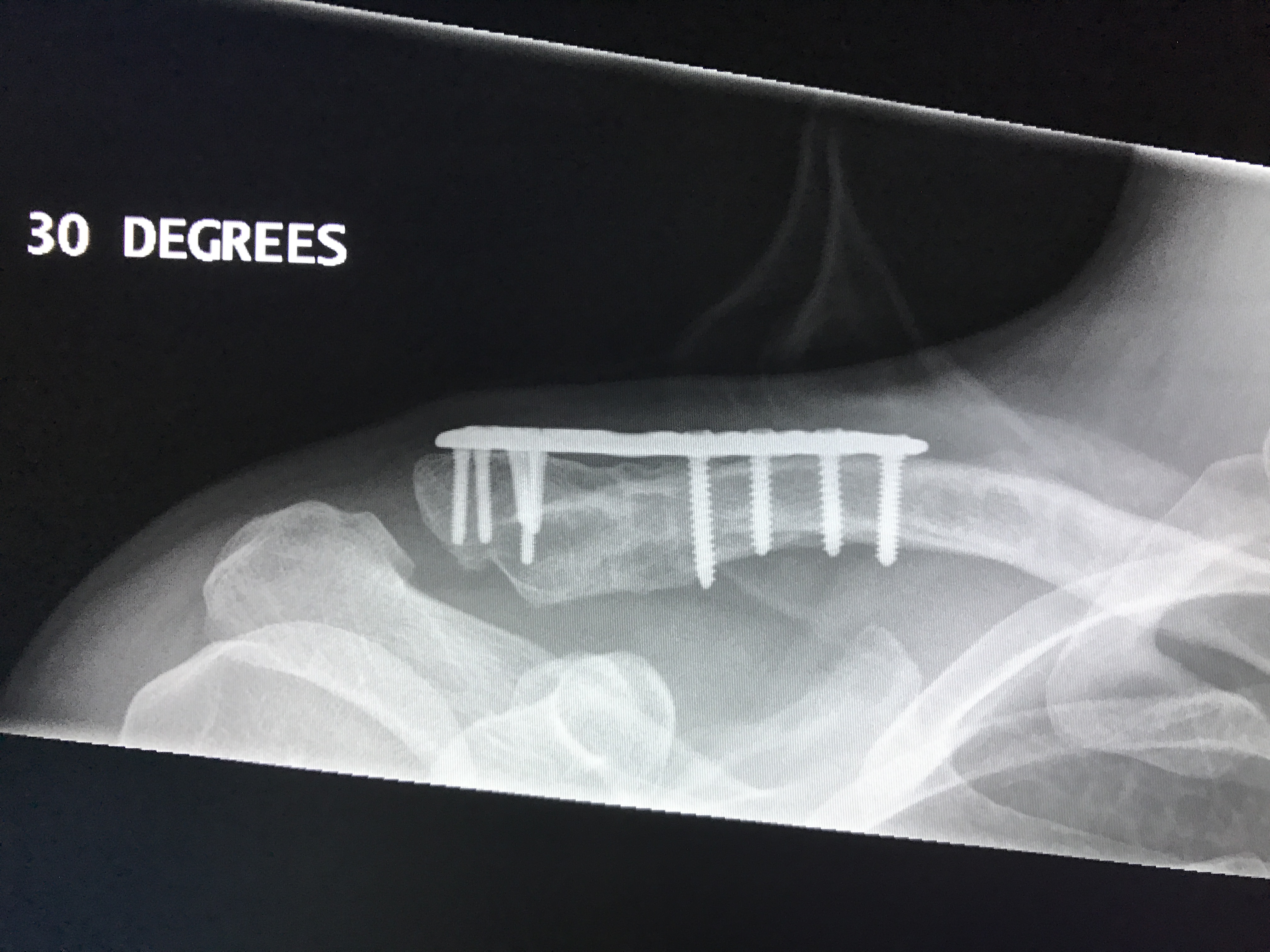
- Stable fixation may be accomplished via the use of the following:
- Plate fixation: subcutaneous location may result in prominence of hardware.
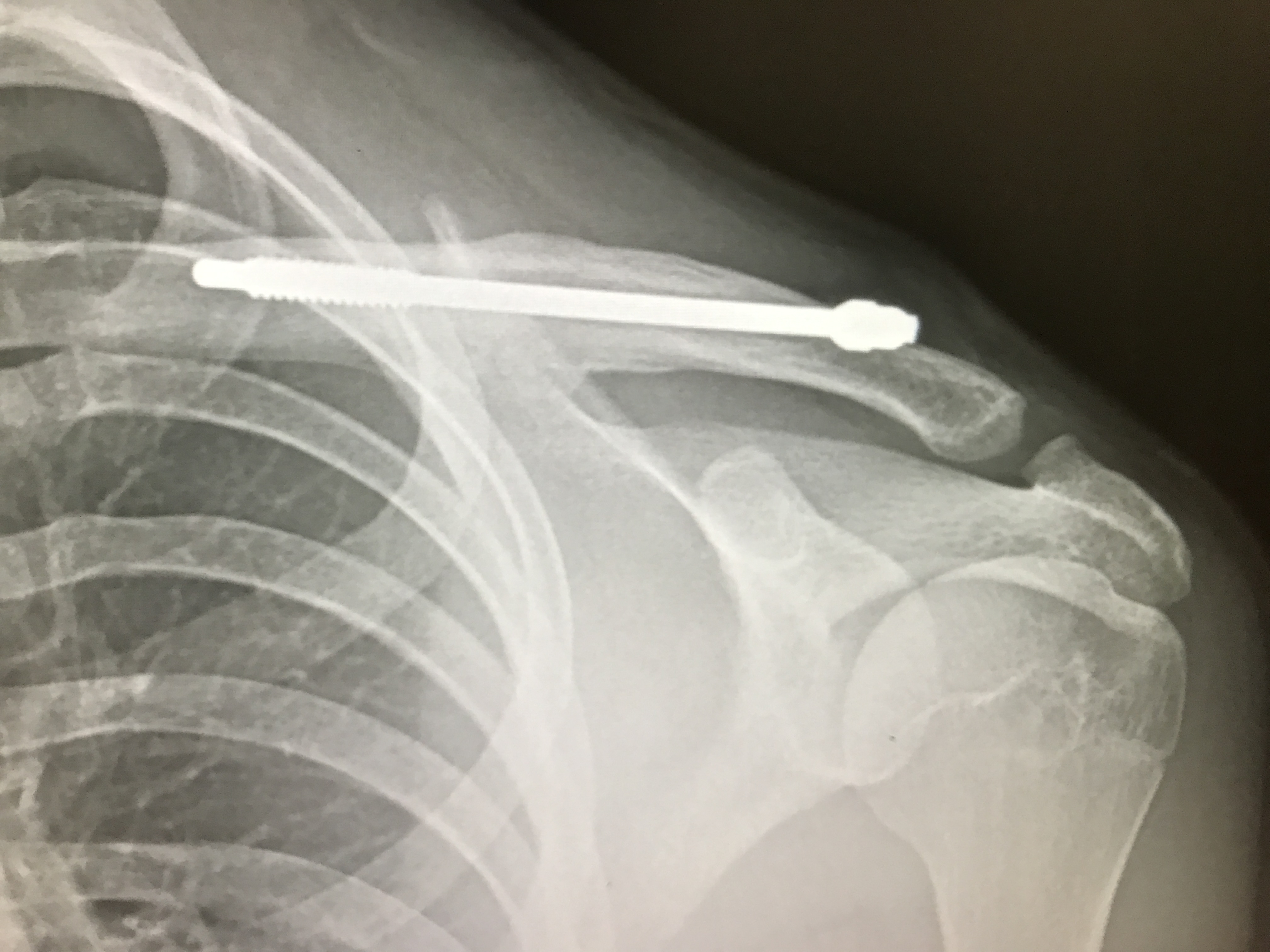
- Intramedullary devices (Hagie pins, Steinmann pins): may be prone to migration of hardware.
- Cerclage suturing or wiring.
- External fixation (Hoffman device).
Rockwood Pin Fixation
Complications
- Neurovascular: laceration of subclavian vessels and brachial plexus; exuberant callus may form in middle third, causing neurovascular compression.
- Malunion: may cause unsightly prominence, but operative management may result in unacceptable scar or painful nonunion.
- Nonunion: rare; predisposing factors include the following:
- Inadequate immobilization (multiple injuries);
- Operative treatment;
- Group II, type II fractures;
- Soft tissue interposition.
- Posttraumatic arthritis: may occur after intraarticular injuries to the sternoclavicular or acromioclavicular joints.
