Minimally Invasive Spine Surgery
Spine surgery is traditionally done as "open surgery." This means that the area being operated on is opened with a long incision to allow the surgeon to view and access the anatomy. In recent years, however, technological advances have allowed more back and neck conditions to be treated with a minimally invasive surgical technique. Typically minimally invasive spine surgery (MISS), does not involve a long incision, it avoids significant damage to the muscles surrounding the spine.
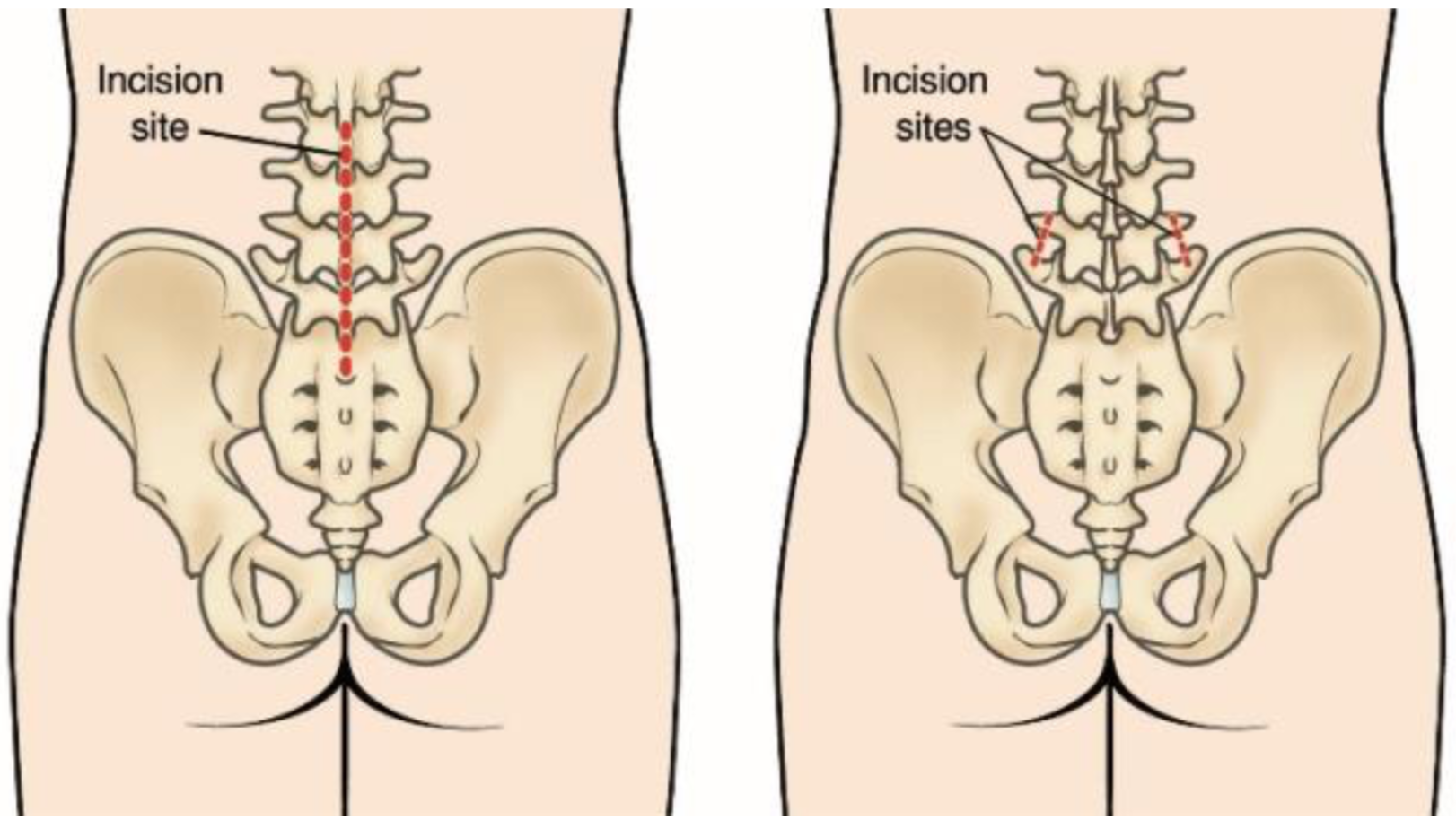
(Left) The incision site in the lower back that is used for some traditional open spine surgeries. (Right) The minimally invasive incisions typically used for a lumbar spinal fusion. Both the decompression and the placing of screws and rods are accomplished through these small incisions
- Better cosmetic results from smaller skin incisions (sometimes as small as 2 centimetres)
- Less blood loss from surgery
- Reduced risk of muscle damage since less or no cutting of the muscle is required
- Reduced risk of infection and postoperative pain
- Faster recovery from surgery and less rehabilitation required
- Diminished reliance on pain medications after surgery
How Minimally Invasive Spine Surgery Works
Because the spinal nerves, vertebrae and discs are located deep inside the body, any approach to gain access to the spinal area requires moving the muscle tissue out of the way. In general, this is facilitated by utilizing a small incision (s) and guiding instruments and/or microscopic video cameras through these incisions. Contrary to popular belief, lasers are very rarely used in MIS surgeries.
Methods:
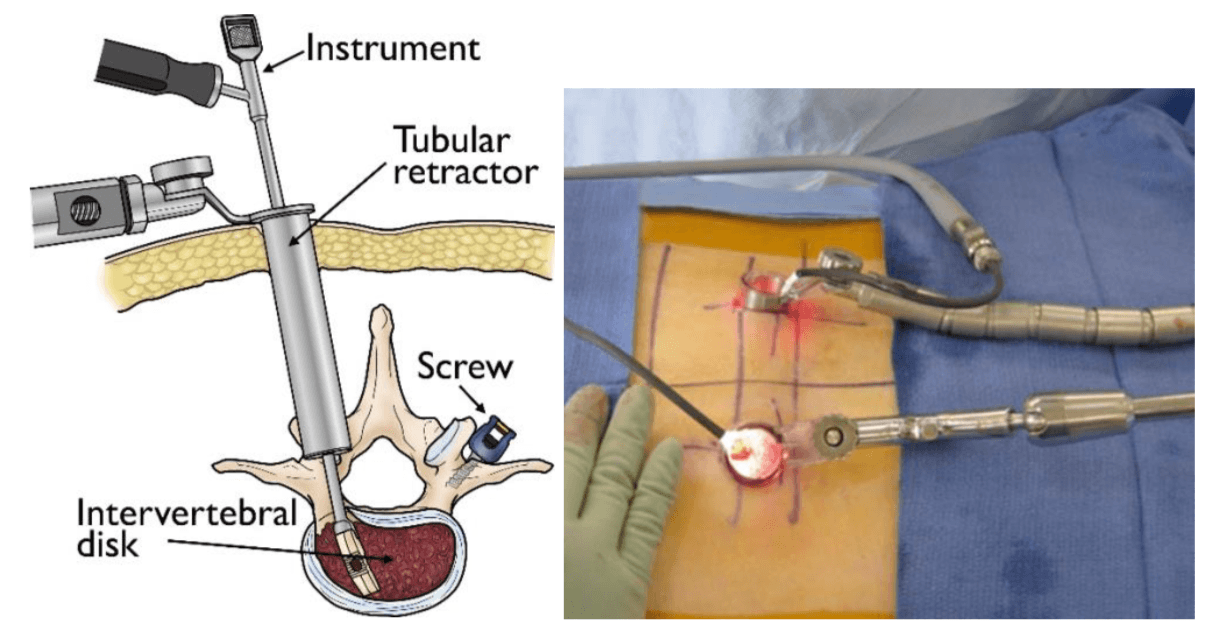
Performing the surgery using a tubular retractor:
This technique involves progressive dilation of the soft tissues, as opposed to cutting directly through the muscles. By using tubes to keep the muscles out of the way, the surgeon can work through the incision without having to expose the area widely. Sometimes, the surgeon will also utilize an endoscopic or microscope focused down the tube to assist with performing the surgery through a minimal access strategy. Once the procedure is complete, the tubular retractor can be removed, allowing the dilated tissues to come back together. Depending on the extent and type of surgery necessary, incisions can often be small.

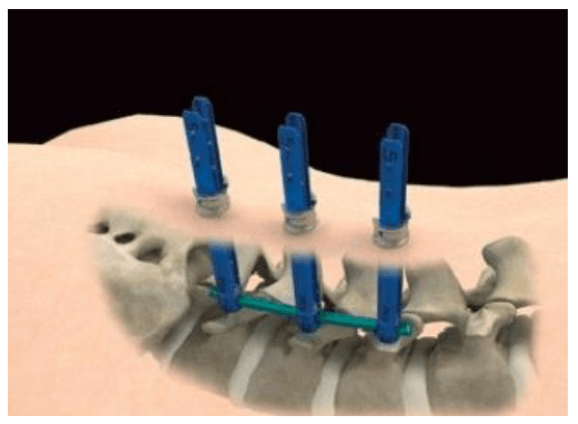
Percutaneous placement of screws and rods for lumbar fusion:
Depending on the condition of the patient, it may be necessary to place instrumentation, such as rods and screws, to stabilize the spine or to immobilize the spine to facilitate fusion of the spinal bones. Traditional approaches for placement of screws requires extensive removal of muscle and other tissues from the surface of the spine.
However, percutaneous (which means “through the skin”) placement typically involves inserting rods and screws through relatively small skin incisions without cutting or dissecting the underlying muscle. With the aid of X-ray images, guidewires are placed through the skin and into the spinal vertebrae along the desired paths for the screws. Then, screws are placed over the guidewires and follow the path of the wires. These screws have temporary extenders that extend outside of the skin and subsequently removed after helping to guide passage of rods to connect and secure the screws.
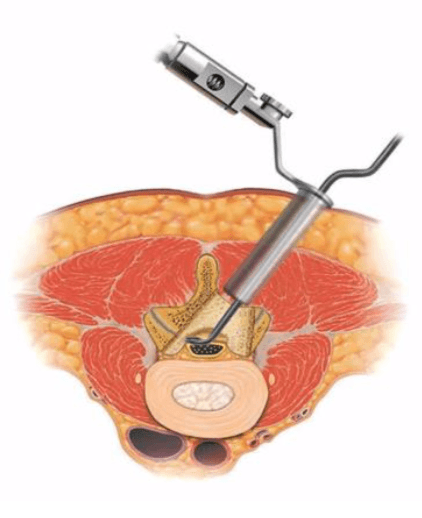
Direct lateral access routes:
In some cases — especially those involving the lumbar spine — approaching the spine from the side of the body results in reduced pain, due to the limited amount of muscle tissue blocking the way. This approach is typically performed with the patient on his or her side. Then, a tubular retractor docks on the side of the spine to enable access to the spine’s discs and bones.

Conditions Treated Using MIS Procedures
- Herniated disc
- Lumbar spinal stenosis
- Spinal instability
- Vertebral compression fractures
- Spinal infections
- Spinal deformities such as scoliosis
- Spinal Tumors
Common MIS Surgery Treatment Options
A number of specific techniques have been deployed for MIS surgery. Though the field continues to develop, the list below highlights some of the most common options:
Discetomy: Spinal discs are essentially elastic rings with soft material inside that serve as cushions between the vertebral bones. If the elastic ring becomes incompetent or weakened, the soft tissue inside can extrude — or herniate — outside of the elastic ring. The herniated disc material can compress the nerves passing by, thus causing pain. If surgical treatment is recommended to trim or remove the herniated disc, it may be possible to perform this procedure with MIS surgery using tubular dilators and a microscope or endoscope.
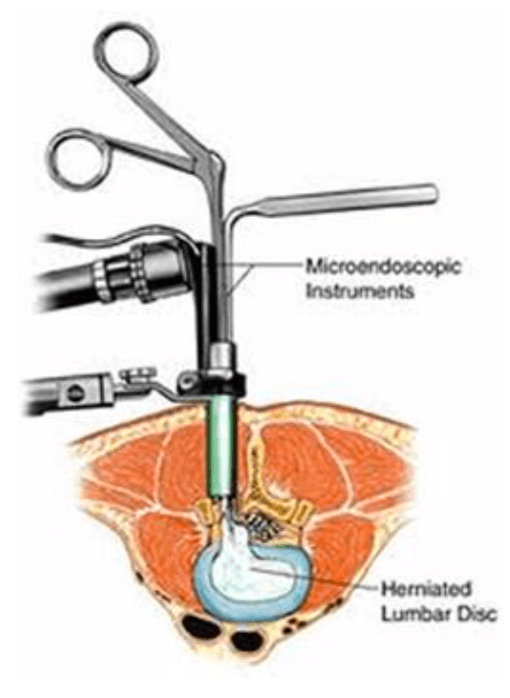
Spinal decompression: Spinal stenosis, which is a narrowing of the vertebral column, is a common condition that can result in compression of the nerves. This can produce a variety of symptoms, including pain, numbness and muscle weakness. If surgery is recommended, it may be possible to remove the bone and soft tissues causing the nerve compression through an MIS approach using tubular dilators and a microscope or endoscope. The more common decompressive procedures include laminectomy and foraminotomy.
MIS TLIF (Transforaminal lumbar interbody fusion): This is a MIS technique that is performed in patients with refractory mechanical low back and radicular pain associated with spondylolisthesis, degenerative disc disease and recurrent disc herniation. The TLIF approach may also have potential in patients with low back pain caused by postlaminectomy instability, spinal trauma or for treating pseudoarthrosis. The procedure is performed from the back (posterior) with the patient on his or her stomach.
Risks of Minimally Invasive Spine Surgery
Any type of spine surgery offers potential benefits and risks—complications can occur. Listed below are several possible complications that may occur during and/or after spine surgery—both open and minimally invasive spine surgical procedures.
- Bleeding
- Blood clots
- Nerve damage causing paralysis and bladder, bowel weakness
- Scarring around the nerves leading to return of symptoms
- Failed fusion (known as pseudo-arthrosis or non-union)
- Failure of metal work
- Infection
Are You a Candidate for MIS Surgery?
Minimally invasive spine surgery offers many benefits: smaller incisions, less pain, fewer risks, and quicker recovery times. However, MISS is still a surgical procedure. Keep in mind that less than 5% of people with back or neck pain need spine surgery — and, surgery should be the last resort for treating pain caused by a spinal disorder.
If non-surgical treatments, such as medications, physical therapy, and/or spinal injections do not effectively reduce symptoms in 3 to 6 months, then you may be a candidate for spine surgery.
Of course, certain types of spinal disorders warrant urgent or immediate surgical intervention. Talk openly with your spinal surgeon about your pain and symptoms, along with the results of different therapies you’ve tried. There are many considerations you and your surgeon need to discuss before making a surgical decision to treat back or neck pain — and if minimally invasive spine surgery may be an option for you.
